Stand up for the facts!
Our only agenda is to publish the truth so you can be an informed participant in democracy.
We need your help.
I would like to contribute
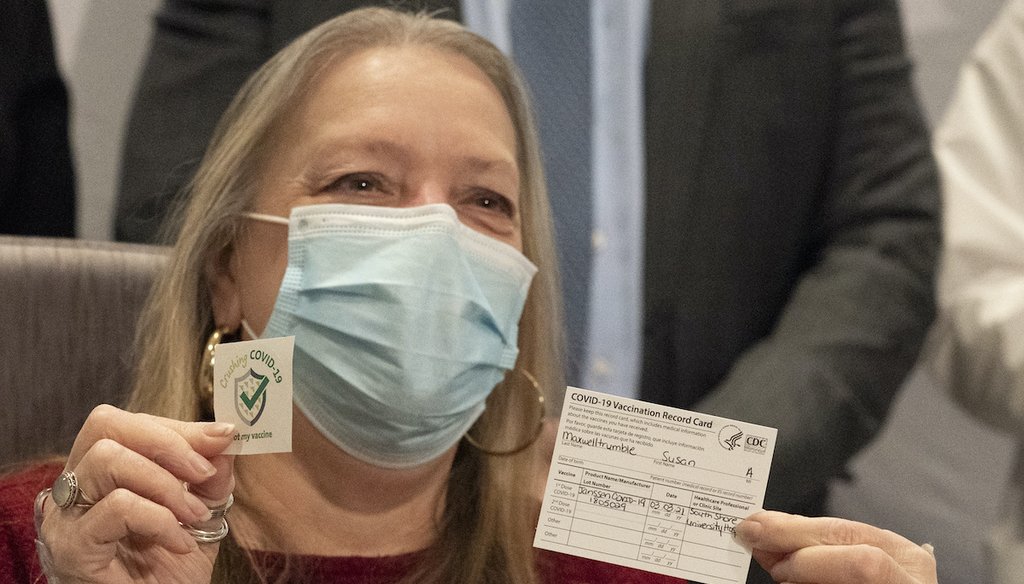
Susan Maxwell Trumble displays her vaccination card after being inoculated with the Johnson & Johnson COVID-19 vaccine at South Shore University Hospital, March 3, 2021, in Bay Shore, N.Y. (AP)
If Your Time is short
- Researchers developing the COVID-19 vaccines were not starting from scratch. The mRNA technology used to create the Moderna and Pfizer-BioNTech shots dates to the 1990s. The viral vector platform used in the Johnson & Johnson vaccine was approved for use for other health emergencies such as Ebola.
- Experts point out that roughly 90 million Americans had received these vaccines as of late March without the emergence of serious safety concerns.
Question: How can the COVID-19 vaccines be safe when they were developed so fast?
Answer:
The development of the first vaccines may have seemed to occur at a dizzying pace. After all, scientists identified a new virus and created vaccines to protect against its most severe effects within a year.
But the research underpinning these vaccines isn’t that new at all, vaccine experts say. Some of it is decades old. This foundation, combined with technical expertise, urgency and financial resources, enabled scientists to pull off the medical marvel.
"The reason it was so fast is money and work," said Dr. Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
COVID-19 mRNA vaccines use the human body’s natural immune response to its advantage. The shot contains the recipe for making the molecule known as the spike protein, which the COVID-19 virus uses to bind to cells. Once the cell receives these instructions, it creates the protein and displays it on its surface. The immune system then spots the unknown protein and makes antibodies to fight it.
The vaccines made by the companies Pfizer-BioNTech and Moderna use this technology, which stems from research that began in the early 19’90s, said Dr. Drew Weissman, a professor of medicine at the University of Pennsylvania. It has been tested against other viruses like influenza. Scientists learned from previous clinical trials and have since worked to perfect the use of mRNA, he said. Previous work on related coronaviruses like SARS helped speed the process.
Weissman and his colleague Katalin Karikó, a senior vice president of BioNTech, are credited with the breakthrough discovery that enabled these vaccines to be safe and highly effective.
"This isn't new technology," Weissman said.
The third vaccine being distributed in the United States to protect against severe COVID-19 uses viral vector technology to generate an immune response. It contains a weakened form of a different virus that carries instructions for cells to make the spike protein found on SARS-CoV-2, the virus that causes COVID. The protein appears on the cell’s surface, and the immune system creates antibodies against it.
Like the mRNA vaccines, this technology carries the code for making the spike protein to the cell, said Dr. Ruth Karron, director of the Center for Immunization Research at Johns Hopkins University.
"The truck is different," she said, "but what's being delivered is very similar."
Viral vector technology has been studied since the 1970s. These vaccines have been approved for use around the world to immunize people against Japanese encephalitis. Johnson & Johnson, which uses this platform for its COVID shot, also created a viral vector vaccine for Ebola after a massive outbreak of the disease in 2019 in the Democratic Republic of the Congo.
In addition to existing research, generous resources were allocated to quickly create the COVID vaccines, experts said. As of December. 2020, the federal government spent $12.4 billion alone on Operation Warp Speed to hasten vaccine development. Drug companies partnered with the National Institutes of Health to tap into its expertise and quickly enroll trial participants.
Perhaps most important, the final clinical trials for the COVID vaccines enrolled between 30,000 and nearly 45,000 participants.
"These studies are so much bigger than the studies we do for many licensed vaccines," Karron said. Some trials for previously approved vaccines have included as few as 3,000 participants, she added.
Dr. Scott Ratzan, who runs a COVID-19 vaccine communications initiative called CONVINCE USA at the City University of New York, said pushing certain information has helped assuage fears among the vaccine hesitant. These include highlighting the reality of the virus, comparing the shot’s side effects to other vaccines and showing the vaccines’ effectiveness in millions of people.
Waiting for others to get the shot first was "a fair thing" when they first rolled out, Offit said. However, after nearly 90 million people in the United States have received at least one vaccine dose with no sign of safety issues, he said, the skepticism should be fading away.
"You have your proof in terms of efficacy and safety," Offit said. If you are still refusing, "then that’s because you’re not a skeptic anymore. You’re a cynic."
Our Sources
Telephone interview with Dr. Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, March 23, 2021
Telephone interview with Dr. Ruth Karron, director of the Center for Immunization Research at Johns Hopkins University, March 24, 2021
Telephone interview with Dr. Drew Weissman, a professor of medicine at the University of Pennsylvania, March 24, 2021
Telephone interview with Scott Ratzan, executive director of CONVINCE USA at the City University of New York, March 24, 2021
Moderna, "Moderna Announces Positive Interim Phase 1 Clinical Data Demonstrating First mRNA Vaccine Candidate, mRNA-1440, Induces High Levels of Immunogenicity," April 27, 2017
National Institutes of Health, "NIH clinical trial of investigational vaccine for COVID-19 begins," March 16, 2020
Penn Medicine, "University of Pennsylvania mRNA Biology Pioneers Receive COVID-19 Vaccine Enabled by their Foundational Research," December 23, 2020
Vaccine, "Live Virus Vaccines Based on a Yellow Fever Vaccine Backbone: Standardized Template with Key Considerations for a Risk/Benefit Assessment," October 27, 2014
Center for Infectious Disease Research and Policy, "Johnson & Johnson's Ebola vaccine lands in DRC," November 4, 2019
U.S Government Accountability Office, "Operation Warp Speed: Accelerated COVID-19 Vaccine Development Status and Efforts to Address Manufacturing Challenges," February 11, 2021
CUNY Graduate School of Public Health & Health Policy, "CUNY SPH Launches CONVINCE USA Initiative to Understand and Address Public Concerns about COVID-19 Vaccines," December 2, 2020
Centers for Disease Control and Prevention, "COVID-19 Vaccinations in the United States," Accessed March 24, 2021
Pfizer, "Pfizer and BioNTech conclude phase 3 study of covid-19 vaccine candidate, meeting all primary efficacy endpoints," November 18, 2020
Moderna, "Moderna announces publication of results from the pivotal phase 3 trial of the moderna covid-19 vaccine in The New England Journal of Medicine," December 31, 2020
National Institutes of Health, "Janssen Investigational COVID-19 Vaccine: Interim Analysis of Phase 3 Clinical Data Released," January 29, 2021
Centers for Disease Control and Prevention, "Understanding Viral Vector COVID-19 Vaccines," Updated March 2, 2021
Centers for Disease Control and Prevention, "Understanding mRNA COVID-19 Vaccines," Updated March 4, 2021

























