Before vaccinations were widely available, COVID-19 tests were considered one of the only tools to help control the spread of the coronavirus.
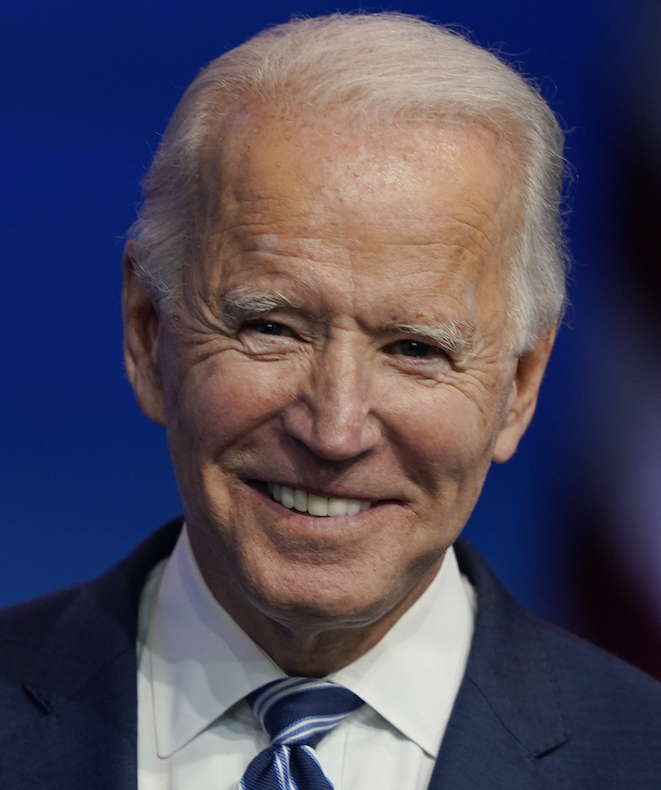
That's why then-candidate Joe Biden promised during the 2020 presidential campaign to boost the U.S.'s COVID-19 testing capacity as one of the ways that he would "beat COVID-19."
Specifically, Biden's campaign website promised that, if elected, he would "double the number of drive-through testing sites" and "invest in next-generation testing, including at-home tests and instant tests, so we can scale up our testing capacity by orders of magnitude."
Now that President Joe Biden has been in office for almost five months, we wondered how he has done? Experts say testing capacity has improved. At the same time, testing demand has decreased and part of Biden's promise — doubling the number of drive-thru testing sites — is harder to pin down.
In February, about a month after Biden took office, his administration announced at a news briefing that it would invest more than $1.6 billion into COVID-19 testing. These funds would, among other things, expand testing in schools and other congregate settings, increase domestic manufacturing of testing supplies and help track new COVID-19 variants via genetic sequencing.
Then, Biden's American Rescue Plan, which was successfully passed through both chambers of Congress in March, also allocated funds specifically to expand COVID-19 testing.
On March 17, the Department of Health and Human Services announced that $10 billion from that legislation would be devoted to screening and testing so schools could reopen, and $2.25 billion to scaling up testing in underserved populations as well as providing new guidance. Another $4.8 billion was allotted in May to reimburse health care providers for testing uninsured individuals for COVID-19.
Dr. Marcus Plescia, chief medical officer of the Association of State and Territorial Health Officials, the organization representing state public health agencies, said that states have begun to receive their American Rescue Plan funds and are starting to plan how testing will be implemented to help schools conduct classes in-person in the fall.
But whether Biden was successful in doubling the number of drive-thru testing sites is unclear. KHN and PolitiFact asked various testing experts for their take, and they generally said they weren't aware of any data that showed the number of testing sites had doubled. Some hypothesized, though, that this may have been because many public health resources were shifted away from testing sites to staff and to set up vaccination sites once COVID-19 vaccines became available to the public.
"I think states did shift their efforts to vaccination, because that was the move in the spring," said Plescia. But as more people were vaccinated, demand dropped and "if we had those drive-thru testing sites we ended up closing them," he added. "It was a promise we ended up not needing to keep."
Indeed, there have been reports of shuttered testing sites across the U.S. In Florida all 27 state-run testing sites closed at the end of May. Oklahoma also recently closed a mass testing site once demand fell to less than 50 tests per day and, in late May, New Jersey closed the state's first outdoor testing site.
The Johns Hopkins University Testing Tracker shows that testing demand in the U.S. has significantly dropped. In January, about 2 million tests were conducted in a day. In May, that number dropped to about 850,000. This reduction occurred at the same time the number of Americans getting vaccinated is rising and COVID-19 cases and deaths are dropping.
The Centers for Disease Control and Prevention also recently recommended that vaccinated people who have been exposed to someone with COVID-19 no longer need to be tested if asymptomatic, and that vaccinated people can be excluded from workplace testing in most instances.
Still, Plescia thinks that if future outbreaks occur in certain areas and more tests are required, states would be able to scale up to meet the need. Especially because of the increased availability of at-home tests — another Biden focus.
So far, the administration has contracted with several private companies to ensure the production and distribution of both rapid and at-home COVID-19 tests.
Ellume, an Australian diagnostics company, was the first to receive an emergency use authorization from the Food and Drug Administration for an at-home COVID-19 test. In February, the Department of Defense announced it had awarded Ellume almost $232 million to build a U.S. factory and increase home-test production. The contract also includes the allocation of 8.5 million home tests to the federal government, which must be provided by the end of 2021.
Abbott, another diagnostics company, received significant funds from the federal government for tests during both the Biden and Trump administrations. In March, HHS announced that Abbott had received a contract to deliver 50 million of its rapid point-of-care tests to long-term care facilities.
Currently, five over-the-counter at-home tests have been authorized for emergency use by the FDA. In addition to the Ellume and Abbott tests, which provide results at home in 15 minutes, a LabCorp test is also available over the counter, but its results take 1 to 2 days to return.
The increase in supply and decrease in demand could mean that some testing efforts originally envisioned by the Biden administration might not be rolled out, and the U.S. may never get to "orders-of-magnitude" increases in testing, Josh Michaud, associate director of global health policy at the Kaiser Family Foundation wrote in an email.
Overall, though, despite the number of drive-thru or mass-testing sites now closed down, there is now a greater availability of COVID-19 tests. The Biden administration has also provided significant funding towards testing, even if some has been redirected.
"In general I think testing is much better," wrote Jeffrey Schlegelmilch, director of the Columbia University National Center for Disaster Preparedness, in an email. "There are easier-to-access options, and the wait times seem to be much faster for results... There are also more resources available to state and local health departments to perform testing. So I would qualify this as a promise kept."
So would we. We rate this a Promise Kept.