Get PolitiFact in your inbox.
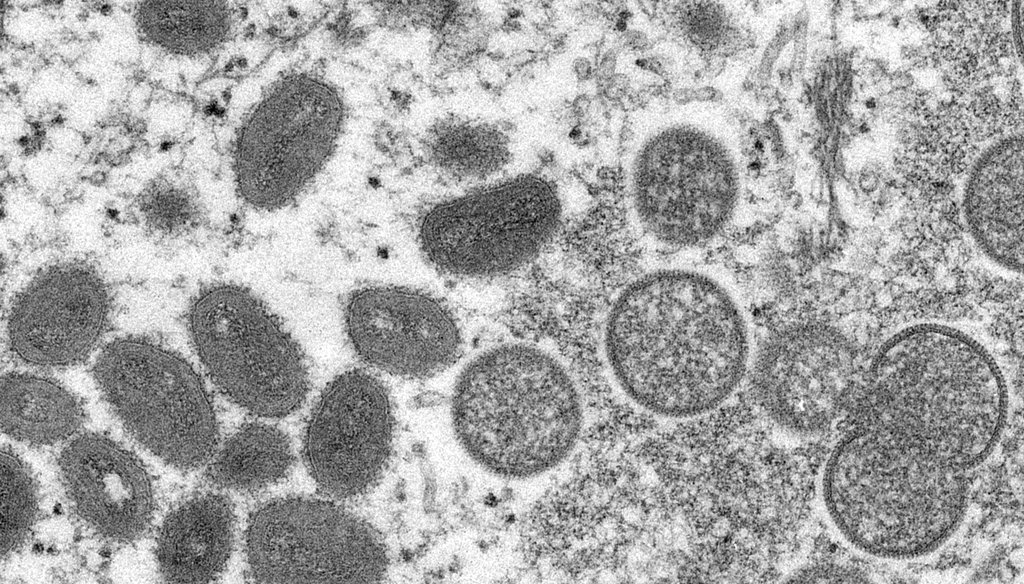
This 2003 electron microscope image from the CDC shows mature, oval-shaped monkeypox virions, left, and spherical immature virions, right, obtained from a sample of human skin associated with the prairie dog outbreak in the U.S.
If Your Time is short
-
More than 250 confirmed or suspected monkeypox cases have been confirmed in at least 16 countries outside of Africa, where it is endemic.
-
Health officials said the virus is mostly spread through direct physical contact with an infected patient. In this outbreak, most of the cases involve men who have sex with men, though it is not a sexually transmitted disease.
-
There are vaccines available, but they are not available to the general public and will be targeted to those most at risk, officials said.
Monkeypox is rarely seen outside of Africa, but a recent spike in cases across the globe has health officials worldwide scrambling to contain the disease.
More than 250 confirmed and suspected cases have been found in at least 16 countries, including the United States and Canada, prompting the CDC to issue an advisory on May 24 urging travelers to take precautions.
The outbreak has already spawned several false conspiracy theories on social media that the outbreak is a hoax, or intentionally created by Bill Gates or others to profit from vaccines or by the government as a biowarfare attack.
President Joe Biden said that while people should be careful, measures like mandatory quarantines likely won’t be necessary in the U.S.
"I just don’t think it rises to the level of the kind of concern that existed with COVID-19," he said, noting that the U.S. has enough vaccines available if needed.
That’s good news for a nation still dealing with a pandemic and recovering from lockdowns and divisions over mask and vaccine mandates. Experts say the disease is not easily transmissible and that vaccines are available, though widespread vaccination efforts are not likely.
Monkeypox is a zoonotic orthopoxvirus with symptoms that are similar to, but less severe than, smallpox, according to the World Health Organization. There are two distinct strains of the virus, Central African and West African, with the former being more severe.
It is endemic in Africa, where it has been steadily increasing in recent years, particularly in Nigeria, "due to a loss of smallpox vaccine-associated immunity" and exposure to infected animals, said David Hamer, a professor of global health and medicine at Boston University Schools of Public Health and Medicine, who is working on surveillance of the current outbreak.
The virus was named monkeypox after it was discovered in 1958 when two outbreaks occurred in colonies of monkeys kept for research, the CDC said. It’s not clear what animal is the original source of the virus, but it is found in many species, particularly rodents, in Africa, the WHO said.
The first case identified in humans was in 1970 in a child from the Democratic Republic of Congo.
It is rare for monkeypox to spread outside of Africa.
As of May 23, there had been at least 70 cases confirmed in England. In the United States, there had been one case confirmed in Massachusetts on May 18 and at least four presumptive cases of orthopoxvirus that were still requiring lab confirmation — one in New York City, one in Florida and two in Utah, the CDC said.
The CDC expects to see more cases in the U.S., said Dr. Jennifer McQuiston, deputy director of the Division of High Consequence Pathogens and Pathology and a captain in the U.S. Public Health Service.
"What's different about what we've been seeing the past two weeks, is that most cases do not have recent travel to Nigeria, or to another country where monkeypox would normally be found," McQuiston said.
Some of the people did travel to Europe and Canada in late April or early May, and the CDC is trying to "connect these dots to determine how the cases are spreading," McQuiston said.
The origin of this outbreak isn’t yet clear, but Dr. David Heymann, an adviser to the WHO, told the Associated Press that it may have been spread by sexual behavior at two recent raves in Spain and Belgium. The CDC said it does not have information yet to tie the U.S. cases to any particular events in Europe.
The CDC said animal-to-human transmission can come from a bite or scratch from an infected animal, direct contact with bodily fluids or lesions, or through touching contaminated fabrics such as clothing and bedding.
Human-to-human transmission can happen similarly — through contact with skin lesions, bodily fluids, contact with contaminated clothing and bedding, or close exposure to respiratory droplets.
McQuiston said people shouldn’t worry about catching the virus from droplets while passing someone in the grocery store, as respiratory spread would require prolonged close contact with an infected person.
"This is not COVID," which we didn’t know a lot about early on, she said. "We do know a lot about monkeypox from many decades of studying it, and respiratory spread is not the predominant worry. It is contact, and intimate contact, in the current outbreak setting and population."
There is no evidence that the virus has mutated and is more transmissible than previous strains, and the sequencing of the virus cases matches what’s been seen in Nigeria in recent years, McQuiston said.
There is no evidence that it is spread through semen or vaginal fluids, experts said. It spreads by skin-to-skin contact, which can occur during intimate sexual encounters but is not exclusive to them. The majority of cases reported in this recent outbreak so far are among gay or bisexual men, but anyone can spread monkeypox if they are in direct physical contact, said Dr. John Brooks, an epidemiologist for the CDC's division of HIV/AIDS prevention.
"Monkeypox is not a sexually transmitted infection in the typical sense, but it can be transmitted during sexual and intimate contact," he said.
Yes, but not usually. In Africa, as many as 1 in 10 people who contract the disease will die, the CDC said. But in most cases, patients recover on their own in two to four weeks without specific treatments. The virus detected in the current spread is the less severe West African strain. That strain has about a 1% mortality rate, Hamer said. There have been no deaths reported in the current outbreak.
Severely immunocompromised patients and those with certain skin conditions like atopic dermatitis and eczema may be at risk for more severe disease, said Dr. Brett Peterson, a medical officer in CDC’s Division of High Consequence Pathogens and Pathology.
There is no specific treatment available for monkeypox that’s proven to work in humans, although there are some antivirals that can be used, the CDC said.
Two drugs, Tecovirimat and Brincidofovir, are FDA-approved to treat smallpox, and the CDC has an investigational new drug protocol to allow Tecovirimat to be used to treat monkeypox. It is seeking the same authority to use Brincidofovir also.
The WHO said patients should let the rash dry if possible, or cover it with a moist dressing to protect the area if needed. They should avoid touching sores in the mouth or eyes, but can use mouth rinses or eye drops as long as they don't contain cortisone.
If you have symptoms or think you may be at risk from a close contact, you should call your doctor to arrange to be tested.
Patients should isolate at home, away from family members, and should only leave home for medical care, the CDC says.
The skin lesions are the most infectious part of the disease. However, because it can be spread by close contact with respiratory droplets, patients should wear a surgical mask around others, as should family members or caregivers who are in close proximity with them for a prolonged period.
There are vaccines available, but don't expect to schedule an appointment for one at your pharmacy anytime soon.
A two-dose smallpox vaccine called Jynneos was approved by the FDA in 2019 for people ages 18 and older who are at high risk for smallpox and monkeypox. It is not available to the general public.
McQuiston said 1,000 doses of the vaccine are available in the U.S. now, and there should be more on the way as the company that produces it, Bavarian Nordic, ramps up production. On May 18, the U.S. exercised a $119 million contract option with the company for a freeze-dried version of the vaccine that would be produced next year.
A spokesperson for the Department of Health and Human Services told PolitiFact that the move by its Biological Advanced Research Authority was not related to the current outbreak. That division works with industry to develop and buy vaccines and treatments for a potential smallpox emergency, some of which can be used to respond to monkeypox, the spokesperson said.
There is also an older smallpox vaccine called ACAM2000 that could be used in people exposed to monkeypox, though it has what McQuiston called potentially "serious side effects."
"A decision to use that widely would have to have some serious discussion behind it. I think right now we are hoping to maximize vaccine distribution to those that we know would benefit from it," McQuiston said. "Those are people who've had contact with a known monkeypox patient, health care workers, very close personal contacts and those in particular who might be at high risk for severe disease."
The WHO said it is working with affected countries "to expand disease surveillance," share information and provide guidance on how to contain the disease.
The CDC said it is working with state departments of public health and other countries to investigate reported cases, and it has alerted medical providers to be on the lookout for monkeypox symptoms. It also said it has worked to speed the sharing of the virus sequencing in U.S. cases with other countries.
Belgium last week became the first country to impose a mandatory 21-day quarantine for monkeypox patients.
It isn’t as easily transmitted as COVID-19. But Hamer said people should be moderately concerned "as this is a relatively contagious virus."
While there is no "great risk" for the general public right now, McQuiston said, it’s important to monitor its movement. "I think that we need to pay close attention to the communities in which this might be circulating so that we can communicate effectively with them and help bring this outbreak under control," she said.
In 2003, there were 47 confirmed and probable cases reported in six states, the CDC said. All of those cases were tied to pet prairie dogs, who were infected with the virus after being kept near small mammals that were imported to the U.S. from Ghana, the agency said.
That was the first time monkeypox was reported outside of Africa, according to the CDC. As a result, the agency issued a ban on importing African rodents that is still in place today.
Aside from that outbreak, the CDC website only lists two single cases of monkeypox in the U.S. involving people who had traveled to Nigeria in 2021.
McQuiston, who is a veterinarian, said there is no high risk to domestic pets. Even in the 2003 outbreak involving pet prairie dogs, there was no spread to domestic animals, she said.
Our Sources
World Health Organization, "Monkeypox"
World Health Organization, "Multi-country monkeypox outbreak in non-endemic countries," accessed May 23, 2022
World Health Organization, "Q&A on monkeypox," May 23, 2022
United Nations, "Bi-Weekly Press Briefing," May 24, 2022
CDC, "Monkeypox in the United States," accessed May 23, 2022
CDC, "About monkeypox," accessed May 23, 2022
CDC, "African rodent importation ban," accessed May 23, 2022
CDC, press briefing, May 23, 2022
Interview with David Hamer, professor of global health and medicine at Boston University Schools of Public Health and Medicine
FDA, "Jynneos"
UK Health Agency, "Monkeypox cases confirmed in England – latest updates," accessed May 24, 2022
The Wall Street Journal, "Smallpox Vaccine Enters Wider Production Amid Monkeypox Outbreak," May 23, 2022
Politico, "Belgium introduces quarantine for monkeypox cases," May 22, 2022
White House, President Joe Biden press conference, May 23, 2022
Bavarian Nordic, "Bavarian Nordic to manufacture first freeze-dried doses of smallpox vaccine upon exercise of contract option by the U.S. government," May 18, 2022



























